Title:
Association between genetic mutations and risk of venous thromboembolism in patients with solid tumor malignancies: A systematic review and meta-analysis.
Introduction:
Venous thromboembolisms (VTE) is a frequent complication in cancer patients with an overall incidence of approximately 20% and is associated with significant morbidity, mortality, and burden on the health care system [1]. VTE risk varies according to tumor type and it is possible that certain genetic mutations may promote hypercoagulability resulting in a prothrombotic state. We have studied the association between genetic mutations and risk of VTE in patients with melanoma, small cell lung cancer (SCLC), non-small cell lung cancer (NSCLC), colon, gastric and ovarian cancers.
Aim:
To evaluate the association of genetic mutations in melanoma, lung (SCLC, NSCLC), colon, gastric and ovarian cancer with the risk of venous thromboembolism.
Search strategy:
We conducted a systematic literature search in MEDLINE and EMBASE electronic databases from inception to May 2020 using a combination of the following subject headings and text words: gene mutation, genetic polymorphism, oncogenes, tumor-related genes, proto-oncogenes, oncoproteins, venous thromboembolism, venous thrombosis, pulmonary embolism, lung neoplasms (SCLC, NSCLC), gastrointestinal neoplasms, ovarian neoplasms, colorectal neoplasms, and melanoma.
Selection criteria:
We included studies presenting data on genetic mutations with > 5% prevalence in our population of interest [adult patients with melanoma, lung (SCLC, NSCLC), colon, gastric and ovarian cancer]. Studies with thrombosis events given, but not listed according to the mutation status of patients were excluded. Retrospective and prospective cohort studies, case-control studies and randomized clinical trials (RCTs) were included.
Data collection and analysis:
General descriptors for the patients in each study were collected, as well as number of patients with wildtype or mutated genes of interest that developed thrombosis. Fixed and random effects models were used to generate pooled adjusted ratios with 95% confidence intervals using data for thrombosis events in patients with mutated and wildtype driver genes of interest.
The quality of the studies:
Study qualities were assessed using Jadad score for randomized controlled trials and the Newcastle-Ottawa Scale for case-control and cohort studies.
Main results:
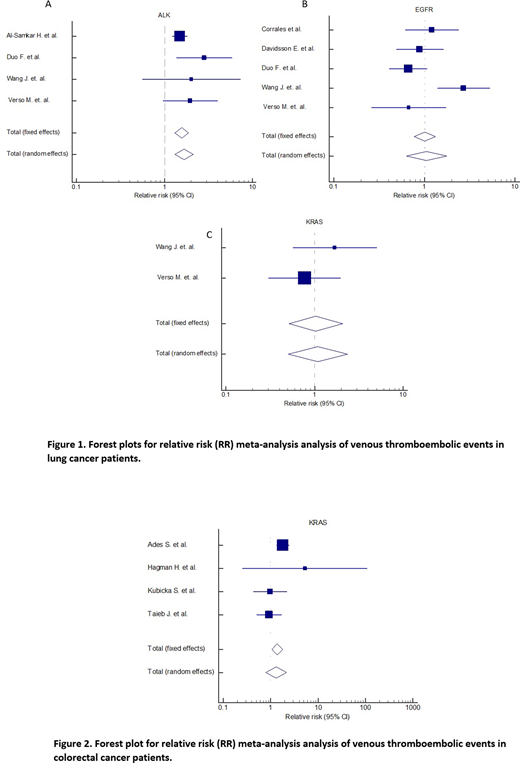
Of 616 eligible articles, we included 31 articles based on our inclusion criteria and 10 were included in the meta-analysis. In patients with lung cancer with EGFR, KRAS and ALK mutations the relative risk (RR) of VTE was 1.006 (40.084-11.150, P=0.965), 1.034 (0.514-2.081, P=0.925) and 1.571 (1.314-1.878, P<0.001) respectively using the fixed-effects model. Using the random-effects model, the RR of VTE in patients with lung cancer and EGFR, KRAS and ALK was 1.058 (0.632-1.768, P=0.831), 1.086 (0.504-2.343, P=0.833) and 1.667 (1.303-2.131, P<0.001), respectively. In patients with colon cancer and KRAS mutation the RR of VTE was 1.38 (1.368-33.942, P=0.017) using a fixed-effects model and 1.319 (0.794-2.191, P=0.285) using a random-effects model.
Conclusion:
In patients with lung cancer, those bearing ALK rearrangements carried a significantly higher relative risk of developing thrombosis than those with wild-type ALK. In patients with colon cancer, relative risk of VTE increased significantly in patients who had KRAS mutations than KRAS wild type.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal